Roman Mars:
This is 99% Invisible. I’m Roman Mars.
Roman Mars:
Imagine for a moment the year 1800, a doctor is meeting with a patient, most likely in the patient’s home. The patient is complaining about shortness of breath, a cough, a fever.
Emmett FitzGerald:
The doctor listens to the patient’s complaints, asks a ton of questions, scribbles some notes.
Roman Mars:
Producer Emmett FitzGerald.
Emmett FitzGerald:
And the doctor might check the patient’s pulse, but unlike today, what’s happening inside of the patient is basically unknowable. There’s no MRI, no x-rays. The living body is like a black box that can’t be opened.
Roman Mars:
The only way for a doctor to figure out what’s wrong with a patient is to ask them.
Dr. Jacalyn Duffin:
You needed the patient to tell you what was wrong and what they were suffering. So doctors were very interested in the patient’s history, the story of what the symptom was, how long it had been there, how had it changed, what made it better, what made it worse?
Emmett FitzGerald:
This is Dr. Jacalyn Duffin.
Dr. Jacalyn Duffin:
I am a hematologist and a historian of medicine at Queens University.
Emmett FitzGerald:
Duffin says that because the patient’s story was all the doctor had to go on, the symptoms were often seen as…
Dr. Jacalyn Duffin:
Diseases in themselves.
Emmett FitzGerald:
So for example, today, if you have a fever, you think of it as a symptom of some underlying disease like the flu. But back at the turn of the 19th century, the fever itself was considered the disease.
Dr. Jacalyn Duffin:
There were all different kinds of fevers and fever itself was a broad category of diagnosis.
Roman Mars:
Because doctors had no way of connecting symptoms with what was actually going on inside the body.
Emmett FitzGerald:
Until someone built a device that would help the doctor open the black box and travel inside the human body. (audio of heart beating)
Roman Mars:
And suddenly the doctor could hear everything so much more clearly. The heart, the lungs, the breath… and everything changed.
Emmett FitzGerald:
The inventor of the stethoscope was, unsurprisingly, a doctor. René Laennec was born in Brittany in 1781, and he went to medical school in Paris where he learned to practice percussion, a technique in which the doctor taps their fingers against a patient’s chest and listens to the sound to determine things like if fluid is building up in the patient’s lungs.
Roman Mars:
Laennec uses the technique for years and in 1816 he’s examining a patient and he percusses her torso.
Dr. Jacalyn Duffin:
But she’s a little bit plump. And because she’s plump, he’s not getting much sound back from percussing.
Roman Mars:
He thought about putting his ear right against the patient’s breast, but he decided that that would be inappropriate.
Dr. Jacalyn Duffin:
So we took a notebook that he had with him and he rolled it up into a little cylinder and he put one end on the patient’s chest and one hand on his ear, and he tells us he was struck by how clearly he could hear her heart beating and her breath sounds.
Narration:
“I was satisfied to hear the beating of the heart in a manner that was clearer and more distinct than I had ever heard it by direct application of the ear.”
Emmett FitzGerald:
He was so impressed by the quality of the sound that he set about trying to construct the perfect device for listening to the internal sounds of the body, all based on that same cylinder shape.
Dr. Jacalyn Duffin:
People said that he became a cylinadromaniac – a cylinder maniac – because he was convinced that the instrument mediating between the two bodies of the patient and the doctor improved what the doctor could hear.
Emmett FitzGerald:
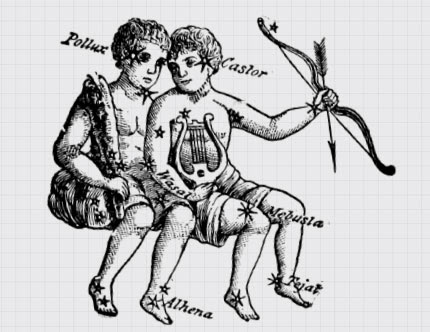
He used a lave to carve cylinders out of wood and at first he wanted to call his new device the ‘cylinder’, but eventually, he settled on the ‘stethoscope’ which means to explore the chest. But Laennec’s original stethoscope looks pretty different from the ones we’re used to today.
Dr. Jacalyn Duffin:
It’s a long tube-like cylinder.
Roman Mars:
It looks like a small handheld telescope.
Emmett FitzGerald:
Laennec started using his new invention to listen to the heart sounds and the breathing sounds of all of the patients in his hospital.
Dr. Jacalyn Duffin:
And he started to invent words to describe the sounds because nobody had heard these sounds before.
Roman Mars:
Laennec had invented a way to hear the inner workings of the human body, but that wasn’t enough by itself. He wanted to connect the sounds he was hearing in his patients with what was actually happening anatomically inside their bodies.
Emmett FitzGerald:
And how do you connect sounds to what’s actually happening inside a body? You listen to people right before they die.
Dr. Jacalyn Duffin:
He ran around the ward listening to all the patients, documenting their symptoms, listening to the sounds they made, and then connecting them to the discoveries he would make at their autopsy when they died.
Emmett FitzGerald:
He thought that every abnormal sound he heard with his stethoscope should correspond to an anatomical finding during the autopsy.
Dr. Jacalyn Duffin:
So that if you hear this sound, it equals that anatomical finding later. So that the stethoscope was a way of practicing the autopsy before the patient became a cadaver.
Roman Mars:
I mean, we’re all just future cadavers, right? But the stethoscope gave us a way of looking inside of a body before it was dead to see what was causing a particular medical problem.
Emmett FitzGerald:
In a relatively short period of time, Laennec made some key discoveries using his stethoscope. For example, he figured out that when a person has fluid beneath their lungs, they make a sound kind of like a goat.
Dr. Jacalyn Duffin:
Kind of a ‘bleating sound’ like this.
Emmett FitzGerald:
A sound he called egophony. He also discovered sounds that tracked with the different stages of tuberculosis, the number one killer in Europe at the time.
Roman Mars:
Laennec published his results, linking different diagnoses with anatomical changes in the body that could be detected using his new stethoscope.
Dr. Jacalyn Duffin:
Doctors who were his colleagues loved it. They felt that every disease would eventually be attached to an anatomical finding and an anatomical change.
Roman Mars:
Some doctors began using Laennec’s new device themselves.
Dr. Jacalyn Duffin:
He even put a diagram of it in his book so you could make your own quite easily or have it made for you by any carpenter.
Roman Mars:
And as these doctors use the stethoscope to make more important discoveries about the body, new categories of disease were created.
Emmett FitzGerald:
For example, before the stethoscope, a lot of different ailments were all lumped into one disease called dyspnea, which means shortness of breath, but after Laennec, shortness of breath became a symptom of various heart or lung problems that could be diagnosed using the stethoscope.
Roman Mars:
Medical language completely changed as doctors invented new anatomical words for diseases like bronchitis, which means the inflammation of the bronchial tubes, the airways that lead to the lungs.
Emmett FitzGerald:
Little by little, our entire understanding of disease shifted. It became more objective.
Dr. Jacalyn Duffin:
Diseases went from being constellations of symptoms felt subjectively by the patient to anatomical or chemical alterations inside the body detected by the doctor.
Roman Mars:
This shift in how people thought about disease changed the relationships between doctors and patients with the doctors suddenly having a lot more power.
Dr. Jacalyn Duffin:
So before the stethoscope, to be sick, you had to feel sick. After the stethoscope, to be sick, the doctor had to find something. It didn’t matter what the patient thought was wrong with them. It mattered more what the doctor found.
Emmett FitzGerald:
Laennec himself actually worried that many doctors were taking his ideas too far. He believed that listening to what patients had to say was still important to understanding disease.
Roman Mars:
But the quest for objective information about disease was underway, and the stethoscope was just the beginning.
Dr. Jacalyn Duffin:
Then we got x-rays, which do the same thing at the end of the 19th century. And now we have CT scanners and MRIs and PET scans, and all of these marvelous devices are basically trading upon the same paradigm that the stethoscope brought along, that we should be able somehow to image the pathological anatomical abnormalities inside the body to reach the diagnosis whether the patient has any symptoms at all or not.
Emmett FitzGerald:
These new technologies have led to so many important discoveries about the human body and disease. Today we can spot tumors before they become life-threatening and diagnose problems like high blood pressure before it causes heart disease. But there are also patients today who struggle because they’ve got tons of symptoms but the doctor can’t find anything, “wrong” with them.
Emmett FitzGerald:
The paradigm shift brought on by the stethoscope has pushed doctors and patients further apart. The doctor is no longer visiting you in your bedroom interviewing you about every tiny detail of your experience. And sometimes patients end up feeling like just a collection of data points rather than a whole human being.
Roman Mars:
René Laennec died in 1826 at the age of 45 most likely from tuberculosis, a disease he and his stethoscope helped us understand. It’s been 200 years since he first rolled up his notebook and pressed it to that patient’s chest. Medicine looks completely different than it did back then, but somehow the stethoscope has endured.
Dr. Andrew Bomback:
There are certain tools of the trade that we have gotten rid of so you don’t really see doctors carrying around this big black bag.
Emmett FitzGerald:
This is Dr. Andrew Bomback. He’s a nephrologist, a kidney doctor, and an assistant professor at the Columbia University College of Physicians and Surgeons.
Dr. Andrew Bomback:
Most doctors nowadays don’t carry around reflex hammers unless they’re neurologists. Most doctors don’t wear that light on their head, but the stethoscope has never really fallen out of practice.
Roman Mars:
But of course, doctors aren’t walking around with wooden cylinders anymore. In the 1840s, they began experimenting with flexible tubing and soon after an Irish physician invented the binaural stethoscope design with two earpieces that we still use. Today, there were a few kinds of specialized stethoscopes for particular types of listening, and more recently companies have developed electronic stethoscopes with enhanced sound quality and the ability to record.
Emmett FitzGerald:
But to this day, when you walk into a doctor’s office for a routine exam, you can expect to feel the familiar stethoscope sliding along your back.
Roman Mars:
But that could be changing.
Archival Tape:
“For almost 200 years, the trusty stethoscope has been at the forefront of the diagnostic procedure, constantly hanging around the necks of doctors and often used, but new technology is threatening to exile this old friend to the archives of medical history.”
Roman Mars:
X-rays and ultrasound have given doctors a clearer window into the body than ever before. And with new portable ultrasound machines, doctors can see an image of a hole in a patient’s heart right from the bedside.
Emmett FitzGerald:
The rise of portable ultrasound has some doctors arguing that we don’t need this stethoscope anymore. They say that if you have that technology, why not use it right away? But ultrasound isn’t available in many developing countries and even in the United States, it’s expensive.
Dr. Dan Bernstein:
Yeah. I mean, if we eliminated the stethoscope and everybody got an ultrasound at every visit, we would bankrupt our healthcare system.
Emmett FitzGerald:
This is Dr. Dan Bernstein, a cardiologist at Stanford University. He says that when he hears something problematic during the stethoscope exam, he immediately orders an ultrasound.
Dr. Dan Bernstein:
But do I start with every patient who comes into the room taking out the ultrasound machine, looking at the lungs? I think that’s not a good use of that technology.
Roman Mars:
Right now he says the stethoscope functions as a screening tool so that patients don’t need to go get an expensive ultrasound unless they need one.
Emmett FitzGerald:
Still, there is no denying that advanced imaging has changed the instrument’s role. Dr Andrew Bomback says that medical students today aren’t as good at listening to the body as they once were. And across the board, doctors rely less on the stethoscope to make a diagnosis.
Dr. Andrew Bomback:
It’s become almost a ritual more than an actual tool of the trade-in terms of helping us make diagnoses.
Emmett FitzGerald:
Recently, one of Dr. Bomback’s most respected colleagues asked to borrow a stethoscope and Bomback was embarrassed because the only one he had with him that day was this cheap plastic disposable thing. But he handed it over anyway.
Dr. Andrew Bomback:
And he said, “Thanks. That’s perfect.” And as he’s walking away, he’s like, “You know, patients just expect you to have this when you see them. I’m not going to really need to use it.” And I thought that was such a funny story because here’s someone that I consider the consummate clinician, and he was acknowledging that the stethoscope was in many ways just sort of a prop.
Emmett FitzGerald:
But it’s an omnipresent prop. If you do a Google image search for doctor, right away you’ll notice a couple of things about what a physician is supposed to look like.
Roman Mars:
Most of the doctor’s pictures on the first page of results are white men in white coats. Some of them are peering inside a patient’s ears, others are writing something down on a clipboard, but all of them have stethoscopes.
Dr. Andrew Bomback:
What I find so intriguing about the Google images searches for doctor is not only is every doctor wearing a stethoscope, but they are almost all wearing the stethoscope in the exact same way, which is like a shawl around the back of the neck
Roman Mars:
With the earpieces on one side and the bell on the other Bomback says that this way of wearing a stethoscope draped over the shoulders is a relatively recent fashion trend.
Dr. Andrew Bomback:
The first time I can remember ever seeing that was on the television show ER and then on Scrubs, which is another very popular medical TV show.
Emmett FitzGerald:
Doctors used to wear their stethoscopes dangling down the front of the shirt, like a tie, and this was practical. If you needed to use your stethoscope in a hurry, you just popped it into your ears.
Dr. Andrew Bomback:
It’s almost like this new version of wearing it like a scar for a shawl, is almost a concession that it’s more fashion accessory than actually a tool that we’re using.
Roman Mars:
But even if the stethoscope exam has become something of a ritual, it doesn’t mean that doctors are ready to give it up.
Dr. Andrew Bomback:
I mean, I would never give up my stethoscope. Because I think in the very least, it’s this conduit to connecting with the patient.
Emmett FitzGerald:
Bomback says that physical contact between a doctor and a patient has become increasingly rare. Doctors’ visits are short and physicians often spend half the time staring at a computer screen. The stethoscope provides an important opportunity for intimacy.
Dr. Andrew Bomback:
The stethoscope is still a part of the exam that is still very much aligned with that idea of the laying on of hands that a healer can do. When we go to do the physical exam, we move away from our desk, we move away from the computer and we stand right next to the patient, and it’s a much more intimate conversation.
Emmett FitzGerald:
And even with all these powerful tools for measuring what’s going on inside a body, intimate conversations are still really important in medicine. Dr. Bomback says he thinks that the stethoscope has come to symbolize to the patient that the doctor is there to listen.
Dr. Andrew Bomback:
And whether we’re actually listening to their heart or their lungs is probably not that important, but what they really want to know is that we’re listening to what they say.
Roman Mars:
200 years ago, Rene Laennec’s invention ushered in a new medical era, one where the patient’s own understanding of their disease gave way to more objective observation of the body. This turn put a certain amount of distance between doctors and patients. Today maybe this stethoscope lives on to keep physicians and patients from drifting too far apart, to make sure doctors keep close to their patients and keep listening.


Comments (11)
Share
“Most of the doctors pictured on the first page of results are white men in white coats.”
That does not even reflect your own screenshot. Why lie?
Every image has someone wearing a stethoscope (the main point), and most are white, most are men and most are wearing white coats. There was certainly no attempt to “lie,” but “most” has been changed to “plurality” to eliminate any ambiguity.
This episode had my eyes rolling out of my head. I am a nurse on a cardiology unit, and I’d like to share a few things that might help round out this episode. First of all, I don’t wear my stethoscope like a damn necktie, because the bell end is a little heavy and would swing around like a mace at pubic bone level. Secondly, I don’t wear it like a shawl to make my patients feel like their medical experience is complete, or because I saw it on ER. I wear it or keep it in my pocket, because it’s comfortable and essential to my job. Some doctors may be losing touch with patients and need some sort of a prop to help bring them closer. Well thank god it’s just a given that your nurse will actually assess you, listen to you, and physically touch you.
We listen to bowel sounds to ensure your gut is working after surgery. We can listen for a fast irregular heartbeat and tell you if that $500 EKG is necessary. We can correlate lung sounds and vital signs and determine in 30 seconds if a patient needs diuretics. We document real-time flowsheets of auditory evidence that guides nursing judgment and decisions. Nurses are constantly using stethoscopes to direct care, so it’s supremely irritating to hear an MD wax on about stethoscopes being some quaint accessory. Doctors ARE using stethoscopes. It’s just via a nurse telling them the patient is drowning in their own fluids, needs more expensive imaging, etc.
“Opportunity for intimacy”?!?! Maybe stethoscopes will become obsolete for physicians because they aren’t using them to good effect. But I assure you, other people are.
*screaming*
This was an outstanding podcast that encapsulates a hot debate in medicine and among medical educators. I am the director of medical education at a US medical school. Our faculty are split between those who believe that meticulous instruction in using a stethoscope (and the physical exam more broadly) is essential to training young physicians. Other faculty — not necessarily younger ones — argue that except for a few gross screening maneuvers, the stethoscope is becoming obsolete and is little better than reading entrails in diagnostic precision.
We all agree, however, that physical contact between patient and physician is essential, and the physical examination provides that opportunity. As importantly, the stethoscope is a symbol of the physician and an important link to its roots. Kudos on illustrating each of these points far better than I’ve stated here.
Anna is obviously right, but she’s younger than me. As someone who was a medical student and intern in the 1970’s..early 80’s I’m one of few people who can tell you about this. Ok, look at Ben Casey the TV show versus ER, the profession of doctor and nurse became way, way grubbier (for nurse, one way). The number of orderlies (CNA’s, now) plummetted and Anna and I became orderlies during the same period. If you were in medical training about 1980, how you wore the stethoscope was a THING that was commented upon. If you were going to be seen as a more active hands on doctor (and that was considered cool), then you wore it as a shawl. This was a class statement. This was an age statement. Older, richer, established doctors wore the stethoscope down. During this same period, the shoes we wear changed. We wore scrubs. AND we changed the way we wore the stethoscope because we ran around. Patient transport, collection of lab data, phlebotomy outside of regular hours and a host of new actually skilled procedures…all the intern/medical student and sometimes nurse.
(oh yeah, and the respect of the profession plummeted but I think you can already see that with Anna’s comment. During the same period the AMA came out against the need for higher nursing staffing, training and pay and I quit the AMA in protest).
Thank you for your perspective. I clearly wasn’t around for the shift in stethoscope style in the 80s, but it makes so much more sense with the context you’ve given. I work with many physicians who I deeply respect, and who work extremely hard for our patients, so I hope my comment wasn’t interpreted as a dig toward MDs in general. It was just bizarre and insulting to hear a podcast about a tool I use daily without the word “nurse” mentioned once. I suppose the MD title doesn’t garner the same respect that it used to, but at least they aren’t erased from the conversation completely. I have been a nurse for a few years now, but I am still finding all the 100-year-old doctor vs. nurse baggage and weird power dynamics really tiresome.
Mainly, I think the point should have been made that the roles of doctors and nurses have evolved to accommodate a super complex and expensive acute care population. To that end, nurses really are the “eyes and ears” of physicians who are given far too many patients to assess or keep track of thoroughly. I just think it works better for everyone (especially the patient) to leave the ego at the door and acknowledge each other’s value to the team.
Everything that Anna said, plus…..the fancy word for shortness of breath is dys-pnea not dyp-snea. I’m also a nurse.
I’m a pediatric hospitalist and the stethoscope is indispensable for my practice. It is not a symbol. It is not a fashion statement. It is my single most important diagnostic device.
The most common causes of pediatric hospital admission (asthma, bronchiolitis, and pneumonia) can all be distinguished by a skilled examiner using a stethoscope in about 10 seconds. Radiographs are costly, take time, and expose children to ionizing radiation. Ultrasound is not widely available at the bedside and even for skilled practitioners takes much longer than auscultation (listening with a stethoscope), not to mention it requires slathering gel on your patient.
I certainly don’t speak for all providers and there are many physicians (ophthalmologists, urologists, psychiatrists, physical medicine and rehabilitation, etc.) for whom a stethoscope is generally unnecessary.
I wear mine shawl-style. I find it uncomfortably tight when worn around my neck. This also keeps the bell from hitting my patients.
Would you consider doing an episode on the white coat?
I enjoyed the podcast for the history lesson, but I agree with Anna about modern assessment. I’m a paramedic. We have an ambulance’s worth of equipment, not an office or hospital full of it. We might begin treating a patient in a ditch. A stethoscope is an essential tool, especially with pulmonary (lung) illness or chest injury. In fact, the longer I practice medicine, the more I respect old fashioned tools for understanding a patient. Labs and ultrasounds and other tools are good medicine. But they augment an “intimate” clinical assessment; they don’t replace it. I highly respect doctors and nurses who do a good clinical assessment before extra tests are ordered.
So, I shared this with one of my bosses, a prominent gastroenterologist, and he cried foul! Repeatedly. Counterpoints to the episode: 1) He says he and other New York providers were rocking the slung stethoscope DECADES prior to Grey’s Anatomy; and 2) The switch from tie to shawl had nothing to do with technology, the impending obsolescence of the stethoscope, or style. It had to do with changes in the length of stethoscopes. According to the boss, stethoscopes used to be much shorter. As such, they could easily be clipped around the neck with the business end resting at a functional level just above the waistline. Over time; however, stethoscopes became longer and longer to keep providers’ faces further and further away from a potentially coughing and wheezing tuberculosis cases. Longer stethoscopes could no longer be worn clipped around the neck because longer stethoscopes place the business end well below the waistline. Pause a moment to think that through. Conclusions: MDs got more and more cautious. Stethoscopes got longer and longer. Stethoscopes moved from neck to shoulders for purely practical reasons. He wore it first. He wore it better.
Beautiful analysis. Thanks. Beautifully done.