For decades, society has dealt with people with dementia and other forms of cognitive decline by storing them away in unstimulating, medicalized environments. But around the world, a new architectural movement is starting to challenge that old paradigm. Designing environments where people with dementia can live as normally as possible, until the very end.
For centuries, dementia patients had been sent to poorhouses and jails. But in the 19th century, many were moved to public mental hospitals. But these institutions were designed to contain people, not care for them. Residents lived in crowded, sometimes unsanitary conditions, with limited access to fresh air and loved ones. When public mental hospitals were forced to close, a wave of nursing homes ushered in a new generation of people with dementia with nowhere else to go. Many of these nursing homes echoed the clinical harshness of their predecessors. Staff resorted to physical restraints, antipsychotics and sedatives to deal with patients. And residents could go months or years without stepping outside.
Journalists, politicians and even advocates and loved ones regularly described people with Alzheimer’s as vegetables, as strangers, as shadows — as better off dead. Even sympathetic news reports presented the disease as it is often described: the funeral that never ends. As the terror of Alzheimer’s spread, federal funding for Alzheimer’s research also surged. But that money was almost exclusively invested in finding a cure or treatment for Alzheimer’s — a strategy that hasn’t panned out yet. And while it’d be great to find a cure, very few resources have been used to study the lived experiences of people with the disease, or to improve the spaces they inhabit.
Many people with dementia live in spaces that are not designed with their specific needs in mind. For example: Part of dementia’s progression involves the loss of visual-spatial skills. Studies have shown dementia patients might perceive a flat screen television as a hole in the wall, or a Paisley-patterned rug as a fish pond in the ground. They can interpret their own reflections in windows and mirrors as entirely other people. By and large, these potential hazards aren’t accommodated in the design of dementia care facilities. But in recent years, some exceptions have been gaining attention — living spaces anchored in dementia-friendly design.
When the Hogeweyk opened in the 1970s in the Netherlands, it wasn’t yet the model for dementia-friendly design. It actually started as a stereotypical nursing home. It was five floors high with long corridors locked by keypads. Handrails flanked white walls. Staff dressed in scrubs. Medical needs trumped human ones. But over time, they saw the need for something different. What they envisioned was an approach that optimized environments for people with dementia, instead of imposing a sterile, nonspecific design. Something that prioritizes the needs of dementia patients above all else.
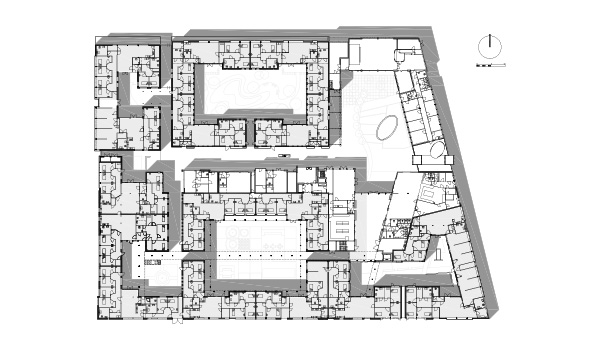
At first, the institution made incremental changes. They swapped out medical furniture for second-hand stuff, and cheerfully decorated the living spaces . They installed a system of doorbells for private rooms and forbade staff from entering until after they’d rung the bell. They shrunk the wards from 30-or-so people down to groups of ten or 11 neighbors.
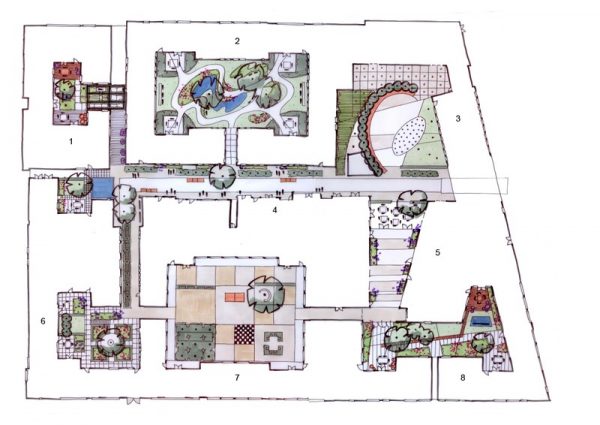
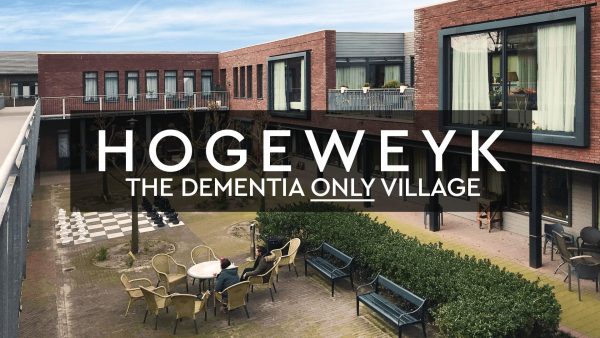
Then in 2005, the Hogeweyk took a big leap forward. They tore down part of the original building and imagined something new in its place. A campus of buildings and spaces made specifically for people with dementia. In 2008, the new Hogeweyk opened. Instead of one big facility, it was a village: a neighborhood of homes, stores, cafes, streets, alleys and parks. Everyone living there has advanced dementia, which means they can no longer live at home alone. And they’re meant to live at the Hogeweyk until they die. But the Hogeweyk does not look or feel like a place of sickness and death. It feels normal — and that’s what’s so unusual about it.
The biggest design innovation at the Hogeweyk isn’t the carpeting or the lighting fixtures, or any advanced medical technology. It’s how the Hogeweyk’s design protects autonomy, and allows people to live the same way they did before the advanced stages of dementia. Every day, for example, someone from each of the 27 homes comes to the Hogeweyk’s supermarket to collect groceries for the daily household meal, which is decided on by the residents. But unlike most grocery stores, there are no price tags, and no money is exchanged at the checkout; the Hogeweyk has conveniently edited out these complicated transactions, so residents can still enjoy grocery runs without worrying about calculating budgets or carrying change.
Of course, the Hogeweyk residents still need careful attention and clinical care. So at any given time, between one and three care workers with medical training watch over each household, helping to lead meal preparation, or washing up. Still, walking around, it’s impossible to tell by the clothes who’s a visitor, who’s a medical professional, who’s a trained volunteer. Everyone is dressed in street clothes: no scrubs, no hospital gowns. The staff are trained not to think of themselves as authority figures who correct behavior and treat symptoms, but to accept residents as they are and work to ensure their happiness.
 Altogether, people living at the Hogeweyk do something that is pretty unusual for people with dementia — they do what people do anywhere. They share meals, make friends, have pets, fall in love. And they develop hobbies! So many hobbies. Near the main plaza, a billboard announces the week’s group activities, like music clubs, gardening, painting, sewing, biking, flower arranging, and happy hours. Smaller groups are more structured, and offer the possibility of making close friends with the same interests.
Altogether, people living at the Hogeweyk do something that is pretty unusual for people with dementia — they do what people do anywhere. They share meals, make friends, have pets, fall in love. And they develop hobbies! So many hobbies. Near the main plaza, a billboard announces the week’s group activities, like music clubs, gardening, painting, sewing, biking, flower arranging, and happy hours. Smaller groups are more structured, and offer the possibility of making close friends with the same interests.
 The design may sound luxurious, and impractical to reproduce. But while Hogeweyk is mainly funded by the Dutch government, it receives the same budget per resident as any other skilled nursing home offering this kind of dementia care in the Netherlands. They just spend that money very differently. Some of those choices come down to the basics that save money on other fronts, like plumbing. Instead of building private bathrooms in every suite, like you’d find in a typical nursing home, the Hogeweyk opted instead for two household bathrooms, similar to what you’d find in a lot of family homes.
The design may sound luxurious, and impractical to reproduce. But while Hogeweyk is mainly funded by the Dutch government, it receives the same budget per resident as any other skilled nursing home offering this kind of dementia care in the Netherlands. They just spend that money very differently. Some of those choices come down to the basics that save money on other fronts, like plumbing. Instead of building private bathrooms in every suite, like you’d find in a typical nursing home, the Hogeweyk opted instead for two household bathrooms, similar to what you’d find in a lot of family homes.
Experts predict the number of people living with dementia will more than double by the year 2050. With this in mind, a lot of people in charge of dementia care are looking to places like The Hogeweyk as a model for how to do things differently — and to treat a person’s social environment as an equally important part of their healthcare.
There are now dozens of dementia villages and senior “microtowns” popping up in countries like Sweden, New Zealand, Canada, Denmark, and Australia. There are no dementia villages yet in the U.S., though one is set to open in New Jersey in the next three years. But there’s not a lot of hope the village model could take off in a big way under a privatized healthcare system. Meanwhile, the Hogeweyk itself continues to evolve. New regulations could allow it to take another radical step forward, by opening the only doors in the village that stay locked to residents: the entrance. That would mean letting residents come and go freely. With these kinds of changes may come risks, but opportunities as well for residents to expand their horizons.





Leave a Comment
Share