Roman Mars:
This is 99% Invisible. I’m Roman Mars.
[MUSIC]
Roman Mars:
Back in the 1960s and 70s, in the city of Pittsburgh, there was a nickname for guys like John Moon — “the unemployables.”
John Moon:
Which simply meant that no matter where you went for a job, nobody would hire you.
Roman Mars:
Moon grew up in Pittsburgh’s largely black and economically depressed Hill District. In better times, the Hill had its own Negro League baseball team and jazz clubs that hosted Duke Ellington and Louis Armstrong. But by the time Moon was graduating high school in the late 1960s, there was no escaping the neighborhood’s “unemployable” stigma.
John Moon:
The reputation was there. The “I don’t want to go to the Hill” because you may get beat up. You have drug addicts and alcoholics. And that same label was placed on myself and I understood that but just because that was your thought doesn’t necessarily mean I had to live up to it.
Roman Mars:
So Moon was glad to land a well-paying job right out of school at the local steel mill, only to discover that the hours weren’t as reliable as he had hoped. Next, he was an orderly at Pittsburgh’s Presbyterian-University Hospital, which provided steady employment, but not much else.
John Moon:
All I was doing was making beds and taking people back and forth to the operating room and lifting and stuff like that, mechanical things where you didn’t have to think.
Roman Mars:
For a while, Moon tried his best to find meaning in the work.
John Moon:
But there was a part of me that said, there has to be something more that I can do.
Roman Mars:
Then one night, halfway through the graveyard shift, Moon watched as two men burst through the doors of the hospital. They were working desperately to save a dying patient. And as they rushed by, Moon stood pressed against the wall and wondered-
John Moon:
Who are these people? What are they doing? How did they get to be able to do that?
Roman Mars:
Maybe today he wouldn’t bat an eye at this scene, but in 1970, nothing about it made sense. The two men weren’t doctors and they weren’t nurses. And their strange white uniforms weren’t hospital issue.
John Moon:
But these guys came in with a certain type of confidence that was just shocking to me from the very point that they came into the room. And they had an emblem on their breast that just piqued my interest.
Roman Mars:
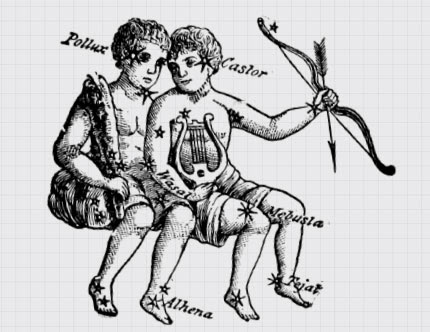
The emblem was the two-snaked Caduceus, the traditional sign of medicine and healing. But just below the familiar symbol was a word John Moon had never seen before — paramedic.
Kevin Hazzard:
Moon wasn’t familiar with the term “paramedic,” because, back then, no one was.
Roman Mars:
That’s reporter Kevin Hazzard.
Kevin Hazzard:
Moon was witnessing the birth of a new profession. One that would go on to change the face of emergency medicine.
Roman Mars:
But to Moon, perhaps the most striking thing of all was that these first-ever paramedics looked like him.
John Moon:
I’m standing here looking at these two guys and I’m saying to myself, “My God, these are black guys.”
Kevin Hazzard:
Never before had Moon seen young African-American men performing that kind of work.
John Moon:
These were two guys that had afros and beards. And the staff on the floor gave them a level of respect that amazed me. And there’s something I never really mentioned to anyone is I actually snuck off of the floor and I actually followed them out to the vehicle because I wanted to see what prompted them to show such proudness and boldness. And once I looked at that vehicle pull off, it was almost like there goes my job, there goes my career. That’s what I want to do.
Roman Mars:
Moon vowed right then, halfway through his long night shift, to become a paramedic… whatever that was.
Kevin Hazzard:
And in Pittsburgh in 1970, the only place to do that was an organization called Freedom House Ambulance Service.
John Moon:
So I went and applied to get a job with them. And the rest is history
Roman Mars:
But that history — about how a group of young black men from Pittsburgh became the world’s first paramedics — is still largely unknown.
Kevin Hazzard:
I’m a former paramedic myself. I did this job for ten years. And you’d think the profession’s origin story would be a big deal. But the truth is, most of the EMTs I’ve talked to have never heard of the Freedom House paramedics — or understand what we owe them.
Roman Mars:
Today, it’s easy to take what paramedics do for granted. Call 911 and they’ll arrive with cardiac monitors, airway equipment, and an array of pharmaceuticals to treat anything from heart attacks to gunshots to premature births.
Kevin Hazzard:
But for a long time, emergency medical service, or what today is called EMS, didn’t provide anything resembling that.
Richard Clinchy:
In the early days of what we would view as EMS, it really wasn’t the equivalent of what we see today. They would do whatever it was they knew to do. But, you know, were they doing the right thing? Who knows?
Kevin Hazzard:
Richard Clinchy is the president of the EMS museum and a trained paramedic. Clinchy says that when he started in emergency care in the late 50s, emergency services didn’t provide treatment at the scene or even necessarily on the way to the hospital. They were just about getting you to the hospital as quickly as possible.
Roman Mars:
Which kind of makes sense in a way. It is, after all, where the doctors are.
Kevin Hazzard:
But, as a result, it often wasn’t clear whose responsibility it was to rush to the scene of an accident.
Richard Clinchy:
Before the evolution of EMS, who did you call? Well, I was a paid firefighter back in the 60s and sometimes we got the call. If somebody needed a fire truck in the city, in New York there were fireboxes everywhere. You’d pull the handle and fire personnel and fire equipment would show up.
Kevin Hazzard:
In other areas, the responsibility for transporting patients often fell to local funeral homes.
Roman Mars:
Imagine that. You’re having a massive heart attack, your life’s in the balance. And who rolls up to save you? Two morticians in a hearse.
Kevin Hazzard:
But in many major cities, this crucial task fell to another municipal service that probably had even less business responding to medical emergencies — the police.
Richard Clinchy:
In the area where I was a firefighter, we had a police department that had a 57 Chevrolet wagon. That was an emergency response vehicle.
John Moon:
So the idea the general public was faced with was more or less what I would call “swoop and scoop,” which simply meant that you’d call the police, they’d rush the person out there to you, and they’d pick you up, put you in the back and rush you down to the hospital.
Kevin Hazzard:
With minimal training and equipment, John Moon says police departments could do little more than offer patients basic first-aid, a canvas stretcher, a half-empty oxygen tank, and a pillow.
Roman Mars:
Which, more often than not, only served to choke off the patient’s airway.
John Moon:
And on top of that, both individuals – meaning police officers – got up front. And left you back there by yourself. So if you stop breathing, by the time you arrived, you were perhaps D.O.A. because no one had done anything for you.
Kevin Hazzard:
The police simply didn’t have the tools, the training or the disposition to save people in a medical emergency, but in the absence of a dedicated emergency medical service, the job was being left to them by default.
Roman Mars:
And perhaps nowhere was the problem of relying on the police for help more vividly illustrated than in Pittsburgh’s largely black Hill District.
Kevin Hazzard:
Moon says the city’s mostly white police force was often slow to respond to emergencies in the Hill. While the black residents, for their part, were reluctant to even call the police to begin with.
John Moon:
Because there was a trust issue with the police, primarily because there were no constraints. They could do whatever they wanted and there was no repercussion or consequences for their actions.
Roman Mars:
No one wanted to get into the exact same police van that the cops had threatened to throw them in the day before.
John Moon:
So there was issues all the way around. Do I really want to call the police? Chances are they’re going to take their time getting here, number one, and if I wait too long, then chances are a cab won’t come to my neighborhood primarily because of fear of being robbed or whatever the case is. So the options were very limited during that time.
Roman Mars:
And the same was true to varying degrees in the rest of the country. Whether a neighborhood was served by the police or the fire department or the local funeral home, so long as the priority was transportation as opposed to treatment, no one even realized there was a “job” that needed doing.
Kevin Hazzard:
But then, in the mid-60s, something happened which flipped the paradigm for emergency care on its head — and laid the groundwork for the invention of paramedicine.
Roman Mars:
In 1966, the federal government published a white paper that would prove so influential that even now in EMS circles it is simply called the “White Paper.”
Richard Clinchy:
Basically, it told us we were killing over fifty thousand people a year on the highways and doing so unnecessarily, that there was a way to intervene and save those people. But we didn’t have the people, nor the resources, nor the training to do a whole lot about it.
Kevin Hazzard:
Techniques practiced by combat medics overseas had been largely ignored by the medical community, with the result that a person was more likely to die of a gunshot wound in America than on a battlefield in Vietnam.
Roman Mars:
The “White Paper” shamed the government into providing money for EMS development on the local level. And government officials and local community leaders began searching for solutions, including a community organizer in Pittsburgh named Phil Hallen.
Phil Hallen:
“Oh, my God. Why do I do this?”
Kevin Hazzard:
Hallen is a former ambulance attendant who came to Pittsburgh in the early 60s and yes, he hates being interviewed.
Phil Hallen:
“Okay, how long are we going to be going on this? I don’t last very long at age 90.”
Kevin Hazzard:
Hallen ran a civil rights organization called the Maurice Falk Medical Fund, which examined health disparities due to institutional racism, and he immediately focused his ire on the city’s pitiful emergency services.
Kevin Hazzard:
“What was your impression of the level of care that was available in Pittsburgh?”
Phil Hallen:
“Well, it wasn’t my impression of it. It was the way it was, you know. There wasn’t any level of care. There was no such thing as emergency medicine or any of the things we now look back on and think what the hell was going on? There was nothing. I mean, nobody was trained. Especially the cops.
Kevin Hazzard:
He could see that what was going on was effectively a public health crisis that was disproportionately affecting black neighborhoods.
Roman Mars:
But then one day, Hallen came across an article in the local paper about a black-operated jobs training program based in the Hill District called Freedom House.
Kevin Hazzard:
The article described how Freedom House had rolled out a kind of mobile grocery store for black neighborhoods, using trucks to bring fresh vegetables to people’s doors.
Phil Hallen:
“Well, health care is terrible in the Hill District. You have to do something. If they can run a grocery van around, why can’t we run a medical van around or something like that?”
Kevin Hazzard:
Hallen wasn’t envisioning anything like modern emergency medical services. At first, he just thought Freedom House’s trucks could help transport people in underserved neighborhoods to the hospital, and that they could hire people from the Hill District to drive them.
Phil Hallen:
“But that’s when I got the director of the University Hospital on this group as well. And, you know, before the first meeting was over, he said, ‘Oh, my God. We have to go immediately to Saffer.’”
[PETER SAFAR: THE EXPERIMENTAL STUDY YOU ARE ABOUT TO SEE IS ONE OF EIGHTEEN SIMILAR STUDIES DURING WHICH WE COMPARED VARIOUS METHODS OF ARTIFICIAL RESPIRATION.]
Kevin Hazzard:
Dr. Peter Safar was the head of anesthesiology at the University of Pittsburgh, and by that time, he was already famous in medical circles.
Phil Hallen:
“Safar was a pure scientist and a very precise and impatient Austrian.”
[PETER SAFAR: WE SIMULATED FIELD CONDITIONS BY SELECTING, AS SUBJECTS, MEN AND WOMEN OF VARIOUS BODY TYPES.]
Kevin Hazzard:
This is a film of Safar from 1951, demonstrating a new technique he developed for resuscitation – what today we call CPR.
[PETER SAFAR: TO HELP ORIENT YOU, WE HAVE MADE A DIAGRAM OF THE EXPERIMENTAL SETUP.]
Kevin Hazzard:
Safar understood that to be effective, resuscitation needed to be started immediately by the first person on the scene. But he faced heavy resistance from the medical community, which felt the general public couldn’t be trusted with such specialized knowledge.
Roman Mars:
So Safar performed an experiment.
[PETER SAFAR: BY ANESTHETIZING AND PARALYZING THESE SUBJECTS, WE SIMULATED LIMP ASPHYXIA VICTIMS.]
Roman Mars:
Safar paralyzed a group of volunteers using a chemical compound from the Amazon normally used on poison-tipped arrows. Let’s just say medical testing has changed a lot.
Kevin Hazzard:
Once the volunteers could no longer breathe on their own, Safar had untrained laypeople use CPR to keep those volunteers alive. And when I say untrained laypeople, I mean children.
[PETER SAFAR: THIS BOY SCOUT WILL PERFORM MOUTH-TO-AIRWAY BREATHING.]
Roman Mars:
Ultimately, Safar’s views would be vindicated, and for his effort, he’d forever be known as the “father of CPR.”
Kevin Hazzard:
Hallen already knew some of this when he walked into Peter Safar’s office in 1966, but nothing could have prepared him for what actually happened.
Roman Mars:
Within seconds of greeting Hallen and the Freedom House team, the wiry and energetic Safar began to unleash a torrent of ideas.
Phil Hallen:
“Basically he said, ‘You are just what I’m looking for. I’ve been trying to figure out how to take rescue breathing and the rest out on the street and to train people how to do that. You’ve got the people.’”
Kevin Hazzard:
But Safar didn’t stop there. He wasn’t content to just teach some van drivers CPR.
Phil Hallen:
“He said, ‘Let’s go beyond that. Let’s train them to be professionals as well. ‘“
Roman Mars:
Professionals who could provide high-quality medical care before the person was even taken to the hospital.
Phil Hallen:
“It was not ‘go to the scene, pick up a patient, transport to a hospital, and then start care.’ It was emergency treatment right there on the pavement.”
Roman Mars:
Instead of repurposed cargo spaces, Safar argued that ambulances should be mobile intensive-care units staffed by professionals trained to use cardiac monitors, administer medication, and anything else that might keep a patient alive.
Kevin Hazzard:
Hallen and the others could barely keep up. Safar wasn’t proposing a simple update to the existing system, but to change the whole culture of pre-hospital care. And he wanted to do it using Freedom House.
Phil Hallen:
“I think somebody said, ‘Well, how big? What are we talking about here?’ He said, ‘I could teach….’ I can remember this. ‘I can instruct 40 people.’ And, you know, and inside of a half an hour, we realized that there was something going on here which was way beyond anything that we had thought of.”
Kevin Hazzard:
Safar set about designing advanced ambulances and an intense 300-hour course, whose graduates would be the world’s first comprehensively trained first responders. This wasn’t just the birth of a profession, but of a whole new branch of medicine. It would become a vital link in the chain, with a subculture all its own.
Roman Mars:
And the world’s first fully-trained paramedics would be staffed exclusively with young black men from the Hill District of Pittsburgh.
John Moon:
And the people that worked there, all were labeled “unemployable.”
Roman Mars:
Freedom House recruited many of its first students right off the street, most of whom were just happy to land a good job, even if they were a little fuzzy on the details.
Kevin Hazzard:
John Moon wasn’t part of that first class. He signed up a little later. But even he admits that as incredible as he thought the opportunity was, he didn’t fully understand what he was getting into.
Roman Mars:
On some level, he was just excited to finally be wearing the uniform with the cool emblem he saw on that first night.
John Moon:
I’ll put it this way, if someone bought you a thousand-dollar suit and just gave it to you and said just walk up and down the street in it, how would you feel? That’s the way I felt. I was at the point where, okay, I got this uniform, that’s all it takes to help people. And boy, was I wrong. It took a little bit more than that.
Kevin Hazzard:
After they signed up, Moon and the others underwent a battery of psychological evaluations and interviews with medical professionals. They learned anatomy, physiology, CPR, advanced first aid, nursing, and defensive driving.
Roman Mars:
At first under Safar, but later under Freedom House’s first medical director — a 30-year-old white doctor with no previous ambulance experience named Nancy Caroline.
John Moon:
And we looked at her with skepticism because, you have to remember, she’s not black. But once we found out that her heart was with us, that was really nothing she could do wrong. And everywhere she went, she took us with her.
Kevin Hazzard:
Caroline got the trainees access to almost every department of the hospital. She had them work in the morgue, the anesthesiology suite, and the maternity ward.
Roman Mars:
And, of course, if they were going to bring the ICU to the street, they had to master everything that happened in an ICU.
John Moon:
So that included spinal immobilization, cervical immobilization, IV insertion. And the advantages of classroom training for us, at that particular time, is we would learn a procedure in class, or she would teach it to us, and then we would go out a half-hour, 45 minutes later after we got a class and perform that procedure on a person.
Roman Mars:
And Freedom House paramedics were often the first people to perform that procedure outside of a hospital.
Kevin Hazzard:
They were among the first to use Narcan to reverse an overdose, and the first to save a patient by shocking their heart in the field. Moon told me that the biggest first he personally experienced came on a call where Nancy Caroline was riding along.
John Moon:
It was a patient having trouble breathing. He was unconscious.
Kevin Hazzard:
So Moon started calling it in. But then Nancy Caroline stopped him.
John Moon:
And lo and behold, she said, “Start an I.V. and intubate this patient.” And I said, “Repeat that?” She says, “Start an I.V. and intubate this patient.”
Kevin Hazzard:
Moon thinks he was the first paramedic who was ever asked to intubate someone in the field. I wasn’t able to confirm that, but intubation — the subtle but critical art of snaking a breathing tube into a patient’s trachea — is an incredibly difficult procedure. I’ve gone through the training. It’s not easy, even in a hospital setting. And here they were doing it on the sidewalk. Moon says he was scared to death.
John Moon:
Once I gathered my nerves together. And remembered how she had taught us in the anatomy lab, I went on and did it. And once intubated the person and I took him to the emergency room, I had to deal with the ER doctor saying, “Well, who intubated this person? Who caused him to be intubated?” And I said, “I did.” “And you are?” I said, “Well, my name is John Moon. I’m a paramedic at Freedom House ambulance service.”
Roman Mars:
But it wasn’t enough for Moon and the other paramedics to simply master the techniques required for emergency medical care. Freedom House personnel faced an even bigger challenge from the moment they got a call.
Kevin Hazzard:
The city had contracted with Freedom House to handle calls in Pittsburgh’s mostly black neighborhoods and the downtown area, but the Pittsburgh police dispatchers often refused to send them.
John Moon:
Because the police looked at us as someone taking their jobs away. Freedom House looked at the police as being a threat to the patient. And one of the things that we had to put in place is we used a police scanner and we would monitor the calls. And we would subsequently try to get to the scene before they did.
Kevin Hazzard:
Moon recalls getting to the scene just seconds after the police arrived and seeing them try to drag patients out of wrecked cars.
John Moon:
And here we are saying, “No you can’t do this. Let’s put him on a spine board and put a cervical collar on them.”
Kevin Hazzard:
But remember these were a bunch of black guys from the Hill lecturing mostly white cops.
John Moon:
And we’re yelling at them and they’re cussing us out.
Kevin Hazzard:
Sometimes the police would relent, but other times they would threaten the paramedics with arrest unless they backed off.
John Moon:
And, you know, the only thing you can do is just stand back and say, okay. And then you watch them, drag the individual out of the car, and put him in the back of a paddy wagon. And both guys get up front and they race off to a hospital. So those were oftentimes battles that you were not going to win.
Kevin Hazzard:
And it wasn’t just the cops who didn’t understand. Patients couldn’t fathom why Moon was using a cardiac monitor and starting IVs in their house instead of hurrying them to a doctor.
John Moon:
Their idea was “let’s call the ambulance, the ambulance comes to pick you up and take you to the hospital.” That’s all they knew. And it wasn’t the easiest thing in the world to explain to a family member that we have brought the emergency room to the person.
Roman Mars:
Trying to convince white patients to submit to treatment was especially difficult. Some wouldn’t even let the Black paramedics touch them.
John Moon:
That was frowned upon on more than one occasion where they would say, “No. Do you have to really do this? I would prefer that you not do it.” It’s something that we had to endure because the problem was not with us. The problem was with the patient. It was their belief or their preconceived notion about the individuals that were touching them.
Roman Mars:
The same went for doctors and nurses at any hospital not directly affiliated with Safar and the Freedom House program.
Kevin Hazzard:
Moon remembers trying to read a patient’s vital signs only to have a nurse laugh in his face, as if he was pretending to play doctor. Other Freedom House paramedics were mistaken for orderlies and asked to mop the floor.
Roman Mars:
But despite all the struggle, Freedom House’s reputation was growing.
John Moon:
People were beginning to recognize that something really different was going on here. This wasn’t just “call the ambulance.”
Kevin Hazzard:
Phil Hallen says stories started to spread about an ambulance service that could perform miraculous life-saving procedures at the scene of horrific accidents.
Roman Mars:
Perhaps the most influential story was about a kid on his bike who was hit head-on by a car. The accident was in Squirrel Hill, one of the city’s most affluent neighborhoods, and one that Freedom House had never been allowed to enter.
Kevin Hazzard:
So initially the dispatcher sent the police. But the cops panicked. The kid was bleeding out in front of them and they had no idea what to do.
Phil Hallen:
“Somebody said, ‘Get Freedom House up here.’ And they did a miraculous activity which nobody had ever seen happen, take place on the street before. People watched it happen. And that was a major turning point.”
Roman Mars:
By this time, Freedom House’s five ambulances were running nearly 6,000 calls a year. And providing demonstrably better care. At a city council meeting, Safar presented data showing that as many as 1,200 people a year had been dying needlessly while in the care of other emergency services. Freedom House paramedics, by contrast, had saved 200 lives in the first year alone.
Kevin Hazzard:
Doctors and medical directors from around the country flocked to Pittsburgh. Freedom House medics were invited to conferences as far away as Germany. Everyone wanted to see what they were doing and learn how they could copy it. And in 1975, the federal government chose Freedom House to field test the first standardized training curriculum for EMS providers. And Nancy Caroline was asked to write the textbook.
Roman Mars:
But Freedom House’s growing reputation would ultimately prove to be its greatest liability.
Kevin Hazzard:
The more successes they chalked up, the more certain residents and city officials wanted to see Freedom House gone. And according to John Moon, it was for a simple reason.
John Moon:
How dare you have an EMS system or an ambulance service this good serving the black economically deprived community – or as society says, “those people” – and we don’t have anything like that?
Roman Mars:
And perhaps no one did more to punish Freedom House for this transgression than Pittsburgh’s mayor.
Kevin Hazzard:
Elected in 1969, 45-year-old Pete Flaherty was a fiscally conservative democrat. Tall and broad-shouldered, he went into office already believing programs using taxpayer money should be managed entirely by the city. But ask Phil Hallen, and he’ll tell you that the mayor’s beef with Freedom House went beyond issues of fiscal or bureaucratic turf.
Kevin Hazzard:
“What was his opinion of Freedom House?”
Phil Hallen:
“Well, he didn’t like it particularly, because it was doing too well and I was black.”
Kevin Hazzard:
“You think that’s why he felt that way?”
Phil Hallen:
“I think so.”
Kevin Hazzard:
“Did… was it your opinion that he was racist?”
Phil Hallen:
“Yes.”
Kevin Hazzard:
When Flaherty took office, he slashed Freedom House’s operating budget in half. This didn’t leave enough money to cover even routine maintenance on the ambulances. Caroline repeatedly wrote frustrated missives to Freedom House’s board, complaining about brakes and steering that locked up, doors that fell from the hinges, and seats that toppled over. Once, according to Caroline, an engine caught fire while transporting a patient.
Roman Mars:
Flaherty passed an ordinance that banned ambulances from using their sirens in certain neighborhoods which significantly slowing their response times.
John Moon:
And at first, they’ll say you can’t use your siren downtown because people are complaining about it. Unfortunately, people look in the vehicle to see who’s driving it and then they complain. So you’re going to a call downtown, you have to blow your horn to tell a car to get out of the way. And they’re looking at you like you’re crazy!
Roman Mars:
Rumors were spread that Freedom House paramedics were selling drugs and running dice games from the ambulances and that thousands of dollars had been stolen from headquarters.
John Moon:
It became a struggle after struggle after struggle and eventually, you know, it’s almost like a patient struggling to breathe, and eventually, the heart gets tired and it stops beating and the person stops breathing and that’s exactly what happened.
Kevin Hazzard:
In 1975, Flattery struck a final devastating blow. He announced that the city would roll out its own brand new paramedic service.
Roman Mars:
Not only was the new service showered with the resources Freedom House had long been denied, its recruits were all white.
Kevin Hazzard:
The city needed Caroline to serve as its medical director and she used that leverage to make one demand—that the Freedom House crews be hired on. Flaherty relented. Sort of.
John Moon:
Because the city was required to bring the employees over but they were not required to keep them. So they found a way to get rid of ‘em. So, you know, that’s how the city’s system ended up being 98% white when the first EMS system in this country was African-American.
Kevin Hazzard:
Within a few years of being replaced by the city’s EMS service, Freedom House was more or less forgotten. In part because, like all good things, paramedics were soon taken for granted. Today, it never occurs to anyone to ask where paramedicine came from.
Roman Mars:
But to Phil Hallen, that’s the true measure of Freedom House’s legacy. Paramedicine is just there.
Phil Hallen:
“Do you know anybody that doesn’t take this for granted at this point in any American city or even in the American countryside? I mean, nobody would even think of a time when somebody would not survive because somebody didn’t know how to do CPR. It’s unthinkable anywhere in the United States.”
Roman Mars:
The model of care created at Freedom House ended up being adopted by countless other paramedics programs across the country, very often with the help of Freedom House veterans. Peter Safar helped to develop a paramedic program in Baltimore. Mitchell Brown, another Freedom House alum, became the EMS commissioner for the city of Cleveland and later its director of public safety. And Nancy Caroline founded the first-ever EMS service in Israel. Her textbook, titled “Emergency Care in the Streets,” ended up setting the standard in EMS instruction for decades.
Kevin Hazzard:
As for Moon, he stayed with Pittsburgh EMS and retired in 2009 as an assistant chief. How does he feel about it all now, when he looks back on the days when a handful of young men from the Hill made history?
John Moon:
It is something I’m extremely, extremely proud to have been a part of and every time I see an EMS unit going down the street, I wonder do they have any idea, that’s where it all began because it all began there.
[MUSIC]
Roman Mars:
Kevin and I discuss what lesson the surprisingly recent history of paramedicine might offer people contemplating a different role for police in our public safety infrastructure today, after this.
[BREAK]
Roman Mars:
Okay. So I’m now talking with Kevin Hazzard, who reported that story for us. And you are a paramedic. I think that’s interesting to note. How did you get into being a paramedic?
Kevin Hazzard:
Basically, after 9/11, I was working as a reporter and, you know, a lot of my friends had been in the military and they had these crazy stories that they would tell. One of them was among the first Marines to enter into Iraq and he’s like cruising along, talking about rockets being fired from a helicopter so close he could feel a heat off of them. And I’m sitting in city council meetings and reporting on whether or not they should put speed bumps in various suburban streets. I was just frustrated and bored. And then one night I got sent by my editor to cover a tunnel collapse. They were doing this huge infrastructure project in Atlanta. And there were six guys on a scaffolding that dropped 250 feet into the earth. We sat outside with the families and waited. And there were a group of paramedics that went down there, sort of high angle rescue team. They rappelled down into the darkness. And we’re all waiting and waiting and waiting. And finally, they emerge. And, you know, of course, the news is as bad as we anticipated it to be. But there was something in those guys in the way that they carried themselves and whatever it was that they saw once they disappeared into darkness of that hole, I just thought, well, whatever version of the truth that I’m looking for, I think those guys are carrying it somewhere within them. So I just signed up for an EMT class completely on a lark. I had no idea if I even could finish it. And next thing you know, I’m sitting on an ambulance and on my way to some ridiculous call. It just all happened somewhat, somewhat accidentally.
Roman Mars:
I mean, it sounds pretty similar to the story that John Moon says, you know, like of seeing someone, being inspired by that as being a vocation and then speaking to you in some way. Did that story have particular resonance with you because of your own experience?
Kevin Hazzard:
Yeah, I did. I mean, if you get to the heart of John’s story, you know, really, he’s a young guy who’s looking for a way to prove himself in the world, particular to a world has ignored him. Obviously, my experience in life is vastly different from John’s. But that to me, it was I saw this group of people who were doing something and I thought that I could do. It didn’t feel like an unattainable goal, but it felt like this incredible opportunity to do this sort of thing that I never anticipated to have the opportunity to do and so there was a lot in John’s story that always felt… that rang true to me.
Roman Mars:
And what part of your career did you learn about this history, about the first paramedics being black men from an underserved neighborhood in Pittsburgh and this whole origin story?
Kevin Hazzard:
No part. I think that’s probably the reason that John sits up a night, you know, filing his teeth in his Pittsburgh home. Nobody knows this. When when I went to paramedic school, my instructors were one of the first six medics in the state of Georgia. And he was telling us these stories of the early days when he was riding a hearse, coming out of the funeral homes and they would embalm bodies one night and then transport the next. And, you know, they’d get a call and you sweep the flower petals out of the back of the hearse and you rush off.
Roman Mars:
So when you see sweeping out petals in the hearse. He was one of those people sent by the funeral home to be an EMS person. Is that is that what you mean?
Kevin Hazzard:
Yeah. And much of Atlanta, the only people who were capable of transporting a body with a funeral house, right? How many people have something like a hearse? And so he was a funeral home employee. And one night a week he would embalm bodies. And then the next night he would be responsible for responding to emergency calls. And this was before there was any notion of a paramedic. So these guys had maybe 10 hours of first aid training. And they’re sitting down in the basement of the funeral home call comes in. They rush out. Again, they yank out the casket, sweep out the flower petals, slide in some sort of a stretcher, and race the streets in a hearse which is these old Cadillac hearses. And he said that if you get going too fast, the brakes would soften up and you couldn’t stop. So they’re screaming in this hearse with a purple light on its roof, screaming through the city of Atlanta with no brakes, flower petals trailing out of the back window.
Roman Mars:
Oh, my goodness. That sounds like a totally different world. It’s amazing that that’s within our lifetimes. That’s just amazing.
Kevin Hazzard:
That’s not that long ago at all.
Roman Mars:
Yeah, yeah.
Kevin Hazzard:
And so hearing these stories of the early days when, you know, they carried a credit card machine with them and before they dropped a patient off the hospital, they’d slide it in front of them and say, “Cash, check or charge.” This really sort of Wild West era in which nobody really knew what they were doing. But that was all I knew about it, was that it started out in a very, you know, slipshod sort of way and then slowly became serious. It wasn’t until after my book came out that somebody said to me, “Hey, there’s another story, another EMS story, if you’re ever looking for one.” And it was set in Pittsburgh. So I started Googling it. And the only thing I could find were a handful of local press accounts of these young men and women who had done this thing in the late 60s, early 70s. And I started digging into it. And all of a sudden the reality of what it was that had happened, that nobody knew. I know a paramedic from Pittsburgh who has no idea that this was the start of it all. And for no one to know that it was shocking to me, particularly someone who did it for a year and wrote about it. When I got in touch with John and I said, “How does nobody know this?” And he just screamed, “I know! Nobody knows!”
Roman Mars:
Oh, I’m so glad that we get to tell the story because it is amazing to me. And it’s pretty resonant today, in particular the role of police in both the story that you told and what’s happening right now. There’s this history there that we presented that is, you know, the police were the kind of default person to be called in this emergency, even though they had no skills or inclination to do the job that was required and we’re looking at what policing means today. And what does it mean that a person potentially armed like a soldier is brought to a situation where someone had a stroke, for example, and maybe that isn’t the right thing to do. And we had this discussion, you know, or we think people had this discussion the late 60s and 70s, too. So when you think about the story you told in your experience, when you think about what the discussions are happening today, how do you take in the moment and reconcile it with this history that we told in this story?
Kevin Hazzard:
Yeah, you know, what’s crazy about that is when I began researching this story, I was coming across quotes that really got to the heart of a conversation we’re just now having today. And these are things that I was reading in the fall and spring of 2018 and 2019. You know, the early medics who were out there saying, “Hey, you know, if you want this police truck to show up at your house, you have to understand that last night that was a truck that showed up to rest your neighbor and tomorrow night might be the truck to show up to rescue you.” And if you really think people are gonna be comfortable calling that guy to arrive tonight then, I don’t think you understand the situation we’re living in. And there was a lot of pushback from the city of Pittsburgh, Allegheny County, about changing this system because it was the system that had always been and people thought, “well, it works,” and somebody was able to come along and prove that, no, this isn’t working. And these guys aren’t suited for this task.
Roman Mars:
No, but I think what is valuable about these lessons of history, it’s so recent that paramedics were invented. It’s so surprisingly recent that it should free your mind to think of the possibilities of what infrastructure, public safety could be today if we didn’t all want it to rest on the police and wanted to try something different.
Kevin Hazzard:
I would agree. I understand the resistance to it. I understand the fear that people feel. When you say something like “defund the police,” it sounds like a really radical term. But if you can sit down and realize how often the police are called out because there’s a psych patient who hasn’t taken his medicine and his 76-year-old parents aren’t certain what to do with them, and this police officer shows up and that’s saying to a hammer, everything looks like a nail. Well, you know, unfortunately, the police really kind of… they’re limited in terms of what they can do. And one of the things I learned very quickly in doing that job was that the police can’t lose a fight. By the nature of their profession, their back is against the wall. And once they arrive, they have to keep pushing forward. And oftentimes that led to a situation that didn’t need to happen. You know, what could have been a situation that we had de-escalated, wound up escalating because the person that arrived was someone who had, essentially, if they didn’t get cooperation, they only had one avenue that they could venture down.
Roman Mars:
It’s amazing to me to think when John Moon saw the paramedics for the first time, he’d never heard the word paramedic. And it was completely novel to most people. And I’m thinking today about how we’re thinking about the police and maybe how to sort of defund them or divest them of some of these activities which they’re not suited towards. I think it’s kind of interesting to imagine that there could be a word, that is like a rapid response social worker, mental health worker that is going to be sent out to people that will be a word like ‘paramedic’ in 50 years. Have you thought about that?
Kevin Hazzard:
It feels like I have. It feels like we’re on the cusp of that moment. There’s no doubt that people are looking for a new way for police to respond. It’s something different to come out and the number of instances we’ve had in which, you know, these situations have gone wrong. How often it has been someone who’s called out for a mental health issue or something that didn’t initially appear to be a crime in progress. And you have to think that somebody out there in the midst of all these “defund the police” conversations, someone must be saying, “Well, how else can we deploy these resources?” Who else can we bring to bear in these situations that can bring a better outcome? And there’s probably a new job title, a new role, a whole new group of people that are sitting out there that not too long from now, we’re all going to look back and say, well, of course, it’s so obvious. Naturally, those guys are there. Naturally, those people are responding. How on earth did we live without them? And I think we’re sort of at the moment where these things are born.
Roman Mars:
Well, I think it’s really interesting. And I am so glad we’re able to share the story. So thanks so much for talking with us and for reporting it. It’s been great.
Kevin Hazzard:
Thank you. It’s really great to be here.
———
Roman Mars:
99% Invisible was produced this week by Kevin Hazzard. Edited by Joe Rosenberg. Mix and tech production by Seira McCarthy and Sharif Youssef. Music by Sean Real. Kurt Kohlstedt is the digital director. The rest of the team is senior editor Delaney Hall, Katie Mingle, Emmett FitzGerald, Vivian Le, Chris Berube, Abby Madan, Sofia Klatzker, and me, Roman Mars.
Many thanks to “The Atavist” for sharing Kevin’s original story with us. If you want to learn more about the history of Freedom House, you should check out that article and if you want to learn more about Kevin’s career as a paramedic, you should go read his memoir. It’s called “A Thousand Naked Strangers.” We’ll have a link to both on our website.
We are a project of 91.7 KALW in San Francisco and produced on Radio Row, which is now distributed in multiple locations around North America, but our heart, it will always be in beautiful downtown Oakland, California.
We are a proud member of Radiotopia from PRX, a fiercely independent collective of the most innovative, listener-supported, 100% artist-owned podcasts in the world. Find us and support us all at radiotopia.fm. Just like these fine people — Emilio Martinez, Ashley Travers, Bill Worthen, Allison Myers, Elizabeth Camero and John and Jen who just got married. Congratulations, and thanks everybody for your support.
You can tweet at me @romanmars and the show at @99piorg. We’re on Instagram and Reddit too. But our true home on the internet is 99pi.org.


Comments (19)
Share
This is one of the best episodes of 99%i out there. Excellent reporting, gripping topic, beautiful storytelling and delivery. Thank you for your hard work Roman & team.
Amazing story. Thank you so much for it!
My sister is a social worker who responds to police calls with (or before) the police when they are called. It is exactly the kind of job Roman was speculating about at the end of the episode. It has been a growing movement in several jurisdictions. My sister works in Utah County, Utah.
This was an amazing story. I grew up partly in Pittsburgh in the 1980s, and I’m ashamed to say that I never heard about this piece of history. Thank you much for such an eye opening piece.
In response to the afterword about possibly having some sort of police-less crisis response: many cities already have this. The longest running is based in Eugene, Oregon called CAHOOTS, but there is even one in beautiful Oakland, CA called MACRO.
Here is a good article about it:
https://www.hcn.org/issues/52.7/public-health-theres-already-an-alternative-to-calling-the-police
CAHOOTS stands for Crisis Assistance Helping Out On The Streets. It started about 30 years ago connected with White Bird Clinic. Peter DeFazio and Ron Wyden are pushing a bill to bring programs like it to other states. Look it up. It includes a licensed social worker, and a paramedic. They work cooperatively with the police. You can thank White Bird and the Buckley House Detox Center for the idea!!! (I’m very proud of my friends who started this program).
Oh, Well. I knew this story. Nancy was a very good friend of my family. Nancy was the mother fonder of EMS and paramedic in Israel. Peter Safar, A great friend. Actually, I find the movie on his experiments in a storage place of MDA – The Israeli EMS. And send a copy to Safar and the museum of anesthesia.
Nancy after retiring from the EMS, started a fellowship in Oncology and established a Hospice in the north of Israel. She wrote a book in palliative medicine. After her early death ( at 55 ) she donates all her books to me and to the Hebrew university. Her picture is on my table. It was a great loss. Her mother died 15 years later at around 95 years old. Thanks for this wonderful story and pictures. When her coffin arrives from Israel to Boston, at the airport a convoy of ambulances with “freedom house” members were waiting for her….
A few moments before the end, there is a discussion of the possibility of, basically, mental health EMS. Well, that very thing is in the works in none other than Alameda County (home of beautiful downtown Oakland California) and will be hitting the streets soon.
I’m disappointed that Roman propagates the confusion between the two-snake Caduceus and the one-snake Rod of Asclepius. I think a correction is warranted.
I agree! 99pi, of all places, should get it right.
Thank you for covering this amazing, inspiring story! It deserves to be better known.
If the streaming services are looking for new material, they couldn’t go wrong to develop a series from this story.
Great show! I heard this not long after listening to a BBC Witness History episode about the invention of the portable defibrillator for heart attacks which also changed procedures for ambulances so that medical care was given at the scene rather than after transport to a hospital, by which time it was often too late: https://www.bbc.co.uk/programmes/w3cszmty
That story should result on a great movie. Netflix, open your eyes!!!
H. James Lucas beat me to it – I’m a few weeks behind on my listening.
In the audio version of this story, Roman speaks of the Caduceus being the traditional symbol of medicine, or something like that. It is anything but, and if you look at the emblems on a modern EMS vehicle, you will see, instead, the Staff of Asclepius.
This confusion became a common feature of American medicine in
the 1900s as the US Army Medical Corps adopted the caduceus as its
symbol.
The original symbol of medicine is the Staff of Asclepius[1], Asclepius being the ancient Greek god of medicine, who was taught the sacred healing ways by Chiron, the
centaur[2]. The myth is that Asclepius had been kind to a snake, who in
gratitude licked his ears clean so that he could understand the snake,
who gave him healing wisdom. Throughout the period some Asclepian
healing temples would allow certain snakes to live in the building and
writhe between the injured and sick. Anyhow, the Staff of Asclepius is
just a walking stick with a single snake wrapped around it.
Contrast that to the caduceus[3]. The caduceus has two snakes wrapped
around a short staff with wings at the top. This symbol comes from
Hermes, the trickster and messenger god (sort of analogous in some ways
to Loki in Norse mythology). The thing is that he’s the god of commerce,
thieves, and fraud. He’s the clever god that’s always deceiving people.
He’s fascinating and interesting but not the connection we should be
lionizing in medicine (although with the way things are going… still,
I’d rather we move back).
Although these have been mistakenly interchanged earlier than the 20th
century, the confusion became a common feature of American medicine in
the 1900s as the US Army Medical Corps adopted the caduceus as its
symbol[4]. I’ve seen it in other countries too but the US is definitely
the worst in getting this wrong. The Medical Corps tried to justify it
on other grounds but I still think it was a poor decision.
[1]: https://en.wikipedia.org/wiki/Rod_of_Asclepius
[2]: Chiron himself has his name immortalized in surgery. One possible
etymology of the world is Chiron –> chirurgeon –> surgeon.
[3]: https://en.wikipedia.org/wiki/Caduceus
[4]: https://en.wikipedia.org/wiki/Caduceus_as_a_symbol_of_medicine
Great story – always learn something new and newsworthy from your podcast. Regarding the final segment of the podcast – check out Cahoots which was founded in 1989 by the Eugene Police Department and Whitebird Clinic.
The measure of a great episode is not only learning something fascinating but also that you can’t wait to tell others what you learned! Hit this one out of the park. While we’re debating Greek, kudos.
Thank you so much for this story. Nancy Caroline was my father’s sister, and listening to this episode, I realized how little context I had for what I knew of her early work. Like so many stories, these were told to me in the framework of family history, so I didn’t know anything about the pioneering nature of Freedom House’s work. Such a delight to stumble over this information!
An interesting story. I am impressed with the drive these people had to advance the treatment of the ill, injured and dying. It is worth noting that training ambulance attendants with medical knowledge is documented back as far as the 1890s in Canada . https://www.ontarioparamedic.ca/before-9-1-1/history-of-paramedics-in-ontario
This is amazing, as a Paramedic from the U.K. I knew some of this history and have taught some of the history of this but I loved every minute of this episode and learned so much new stuff I will include in my teaching, thank you all for doing some an amazing job